Facet Syndrome
What is facet syndrome?
Vertebral facets are where two vertebrae come into contact and form facet joints (or zygapophyseal joints) that link adjacent vertebrae. Facet joints are present in all regions of the spine, in the neck (cervical), mid-back (thoracic) and low back (lumbar). However, facet syndromes are most common in the lumbar and cervical spine and rarely occur in the thoracic region.
Ramsook RR, Bryce TN. Facet-Mediated Pain. 2017
Facets are common sources of pain as they bear heavy loads. There are multiple reasons why facets may cause pain, the most common being: trauma resulting in a sprain (sudden twist, for example), repetitive joint stress causing inflammation, entrapment of joint structures within the joint and age-related degeneration.
Lumbar Facet Syndrome
What are the signs of lumbar facet syndrome?
Low back pain is the predominant feature of lumbar facet syndrome, and it may arise suddenly following trauma or gradually over time. The pain may also radiate into the flank, groin and side of the thigh if the upper back is involved or to the buttock and posterior thigh in case of lower back involvement, but will rarely radiate past the knee.
It is usually aggravated with the extension of the spine (arching of the back) and relieved with flexion (bending forward), although that is not always the case. Patients may have a history of trauma or repetitive bending and lifting.
Diagnosis
Diagnosis is made clinically through a series of orthopaedic tests and observations. An increased lower back curvature (lumbar lordosis) may be noted. In addition, hyperextension of the lower back reproduces local and referred pain. Local muscle tightness and tenderness may be recorded.
No actual neurological signs should be present. However, some weakness may be noted due to pain.
Prognosis
Acute facet syndromes respond well to manual therapy and take an average of 6 to 12 weeks to heal. Chronic cases linked to degeneration have a poorer prognosis. However, they can be managed by regular care and building and maintaining strength in the area.
Treatment Recommendation
There are a couple of reasons why facet injuries can cause significant amounts of pain for patients. Firstly, as the body attempts to heal, inflammation will build up in the area, causing pain and swelling. In addition, entrapment of the joint structures with the spine in extension may generate discomfort. Finally, as a protective mechanism, the muscles supporting the spine will go into spasms to protect the joint. Treatment will therefore aim at addressing all of these components.
Phase 1: Acute Care
In the acute stages of injury, the focus is reducing swelling and inflammation to help the pain. Putting the spine in light traction to increase joint space and placing pelvic blocks under the hips to create flexion will decrease discomfort by reducing the load on the joint. Manual adjustments are used to increase motion and reduce pain. Soft tissue therapy is also essential to soften the muscle spasms in the area.
Phase 2: Stabilisation
The second phase of care aims to stabilise the area by adding rehabilitation exercises to engage the muscles and take pressure off the facet joints. A resilient and robust spine and paraspinal muscles are the best defence against more episodes of facet pain.
Phase 3: Strengthening and Maintenance
Finally, maintenance care helps prevent the risk of re-injury and monitor progression. Strengthening the stabilising spine muscles to correct postural imbalances and anterior pelvic tilt will decrease loading on the facet joints, thus preventing reoccurrence.
Home Advice
In the acute stages, anti-inflammatory medication may help alleviate the pain, and applying heat to the area has been known to help. Movement is recommended, keeping in mind to avoid hyperextension of the spine. In the early stages, avoiding lifting and bending that unnecessarily loads the spine is also recommended. The patient can perform gentle range of motion exercises and stretches favouring flexion.
As we progress to stabilisation, strengthening exercises can be prescribed to increase spinal stability. Progressive loading is critical to restoring correct biomechanics while preventing re-injury.
Give examples of exercises with pictures.
Before attempting these exercises, it is highly recommended to see a qualified chiropractor get a correct diagnosis and treatment plan tailored to your condition.
Acute Phase
Pelvic tilt
Stretch - Qls, psoas, glutes
Leg fallouts + table tops
Light bridges
Stabilisation Phase
Glutes side series
Single leg stretch
Bridging with pulses
Stretch - Qls, psoas, glutes
Strengthening Phase
Hard glutes
Hard lower abs
Bridging with table tops
Increase endurance with exercises
Stretch - Qls, psoas, glutes
Cervical Facet Syndrome
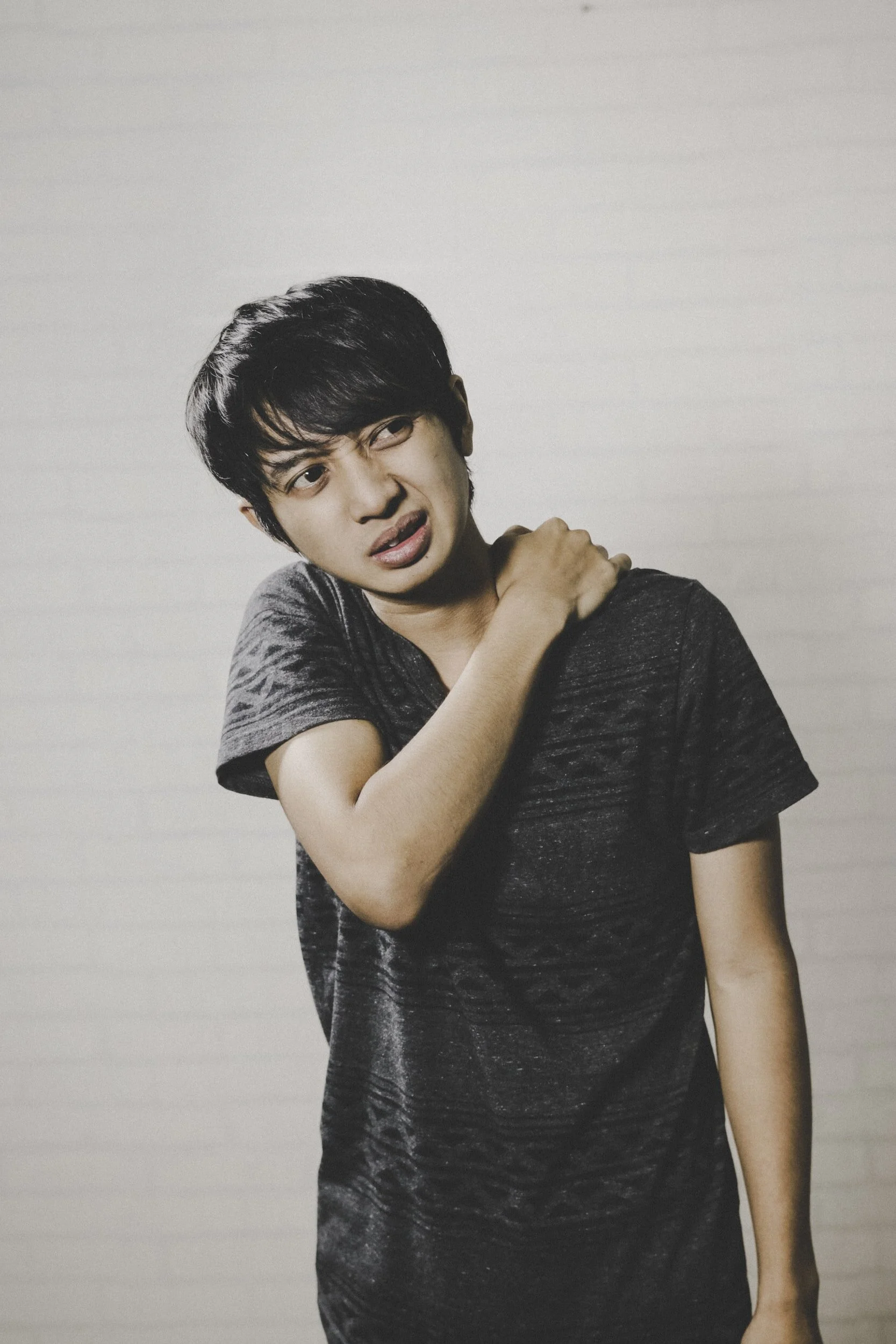
What are the signs of cervical facet syndrome?
Neck pain is the predominant feature of cervical facet syndrome; it may arise suddenly following trauma or gradually over time. The pain may also radiate into the head, upper back and shoulder but will rarely go past the elbow. It is usually aggravated with extension and rotation of the spine (looking up and to the side) and relieved with flexion (looking down), although that is not always the case. Patients may have a history of trauma.
Diagnosis
Diagnosis is made clinically through a series of orthopaedic tests and observations. There is tenderness on palpation of the involved facet, and hyperextension and rotation of the neck reproduce local and referred pain. In addition, local muscle tightness and love may be noted.
No neurological signs should be present; however, some weakness may be noted due to pain.
Prognosis
Acute facet syndromes usually respond very well to manual therapy and take an average of 6 to 12 weeks to heal. Chronic cases linked to degeneration or poor posture have a poorer prognosis; however, they can be managed by regular care and by building and maintaining strength in the area.
Treatment Recommendation
There are a couple of reasons why facet injuries can cause significant amounts of pain for patients. Firstly, as the body attempts to heal, inflammation will build up in the area, causing pain and swelling. In addition, entrapment of the joint structures with the spine in extension and rotation may generate discomfort. Finally, as a protective mechanism, the muscles supporting the spine will go into spasms to protect the joint. Treatment will therefore aim at addressing all of these components.
Phase 1: Acute Care
In the acute stages of injury, the focus is reducing swelling and inflammation to help the pain. Tractioning the spine will increase joint space and reduce the load on the joint. Manual adjustments are used to increase motion and reduce pain. Soft tissue therapy is also essential to soften the muscle spasms in the area.
Phase 2: Stabilisation
The second phase of care aims to stabilise the area by adding rehabilitation exercises to engage the muscles and take pressure off the facet joints. A resilient and robust spine and paraspinal muscles are the best defence against more episodes of facet pain.
Phase 3: Strengthening and Maintenance
Finally, maintenance care helps prevent the risk of re-injury and monitor progression. Strengthening the stabilising muscles of the spine to correct any postural imbalances will decrease loading on the facet joints, thus preventing reoccurrences.
Home Advice
In the acute stages, anti-inflammatory medication may help alleviate the pain, and applying heat to the area has been known to help. Movement is recommended, keeping in mind to avoid hyperextension of the spine. The patient can also perform a gentle range of motion exercises and stretches that favour flexion.
As we progress to stabilisation, strengthening exercises can be prescribed to increase spinal stability. Progressive loading is critical to restoring correct biomechanics while preventing re-injury.
Before attempting these exercises, it is highly recommended to see a qualified chiropractor get a correct diagnosis and treatment plan tailored to your condition.
Acute phase:
Cervical ROM exercises - Start in a seated position looking straight forward.
Look over your right shoulder and hold at end range for a few seconds, then look over the left shoulder and hold for a few seconds. Then take your right ear to your right shoulder, save for a few seconds, and finally, take your left ear to your left shoulder and hold for a few seconds.
Keep your upper chest relaxed and neck and shoulders soft at all times.
Only go as far as you comfortably can without forcing.
Repeat for the desired number of repetitions.
Lightly seated chin tucks (James)
Pec stretch
Light upper traps stretch (without overpressure)
physio ball - blue ball chin tucks
Stabilisation phase:
Chin tucks quadruped
Rotator cuff exercises
Self snags w dressing gown belt
UT Stretching with hand on head (no pulling, just weight of writing is enough)
Pec stretch
Thoracic extension foam roller (hands-on neck for support)
Shoulder rolls
Scap retraction w arm lifts/shoulder abduction
Strengthening phase:
Ball behind neck mini squat (James)
W to V (lower traps)
Dr Elsa de Froberville
BscAnat., BscChiro., BChiro.
Chiropractor | Spine & Sports Centre